
Make peripheral lines a central focus
Request DemoTrained & committed people
Good PIV Catheter care takes training and commitment. Watch these educational courses made to help clinicians ensure proper protocols are followed for every patient, every time. Further educational modules are in preparation in Europe. Keep in touch to know when they become available! Learn more about 3M resources to help clinicians ensure proper protocols are followed for every patient, every time.
Watch these PIV Care education courses
you can watch these modules if you are a registered user of our Healthcare Academy. Get your credentials ready and click here!.
Not registered yet? Get your access to our Healthcare Academy now!
-
Join Whitney Ficocello, BSN, RN, PHN, 3M Technical Services Specialist, to learn about current clinical standards addressing peripheral vascular care, discuss clinical challenges associated with peripheral catheter maintenance, and identify potential solutions to address these challenges.
-
Watch a webinar with Matthew Ostroff, MSN, AGANCP, CRNI, VA-BC, CEN, Vascular Access Coordinator and Lead Clinician at St. Joseph’s Health, to identify current trends in addressing peripheral vascular access care, discuss clinical challenges and evidence-based interventions, and identify potential solutions to address these challenges to improve care for every patient.
-
Learn from Mary Duncan, RN, MSN, CIC. Sr. Director of Infection Prevention, in a free webinar about a new study that showed reduction of primary bloodstream infections (BSIs) by following a Peripheral IV Maintenance Bundle.
-
Learn from 3M Technical Service Specialist Joseph Hommes, RN, BSN, VA/BC, in a free webinar about the impact, incidence, and clinical considerations of peripheral IV complications. Understand how to protect peripheral IV sites and reduce risk of complications.
Our 3M specialists will answer your questions - either in person or with an online consultation and virtual demonstration. We are here for you.
Prevention in practice: PIV care and maintenance guidelines.
We believe having the right standards of care, combined with the latest technology can help improve outcomes for every patient. Review these care and maintenance recommendations from around the world:
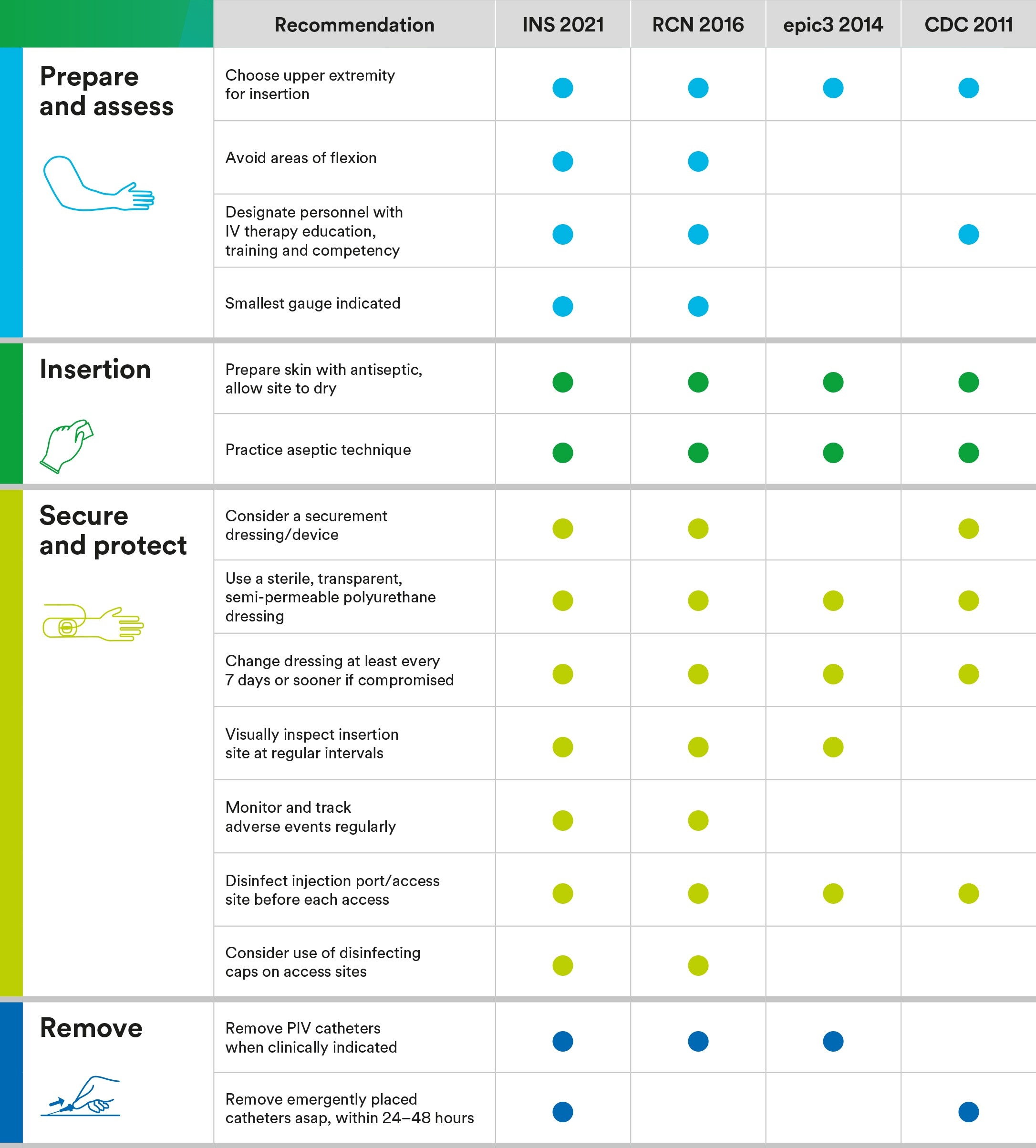
INS 2021: https://www.ins1.org/
epic3 (2014): https://improvement.nhs.uk/documents/847/epic3_National_Evidence-Based_Guidelines_for_Preventing_HCAI_in_NHSE.pdf
CDC 2011: https://www.cdc.gov/infectioncontrol/pdf/guidelines/bsi-guidelines-H.pdf (PDF, 610 KB)
-
Forms a protective film between the skin and the adhesive
-
3M’s packaged single-use length medical tape rolls can help reduce exposure to bacteria and spores ⁸
Effective & proven technology
3M’s evidence-based antimicrobial product offerings protect against both extraluminal and intraluminal contamination of PIVs. When properly deployed, these antimicrobial solutions offer another line of defense against potential contamination.
Resources
-
 Peripheral IV Care Solutions Brochure
Peripheral IV Care Solutions BrochureLearn how to reduce the risk of peripheral IV complications at all access points and make peripherals a central focus of your IV care program.
Our apologies...
An error has occurred while submitting. Please try again later...
Thank you!
Your form was submitted successfully
References
-
- Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(S4):S38–S42.
- Résultats de la surveillance nationale 2019, REPIAS, SPIADI. Accessed February 25, 2022. https://www.spiadi.fr/results?tab=0
- NRZ Deutsche nationale Punkt-Prävalenzerhebung zu nosokomialen Infektionen und Antibiotika-Anwendung 2016 Abschlussbericht, Accessed February 25, 2022. https://www.nrz-hygiene.de/fileadmin/nrz/download/pps2016/PPS_2016_Abschlussbericht_20.07.2017.pdf (PDF, 4.1MB)
- Mermel LA. Short-term peripheral venous catheter–related bloodstream infections: a systematic review. Clinical Infectious Diseases. 2017;65(10):1757-1762
- Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: Peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189–203
- Saliba P, Hornero A, Cuervo G, et al. Mortality risk factors among non-ICU patients with nosocomial vascular catheter-related bloodstream infections: a prospective cohort study. Journal of Hospital Infection. 2018;99(1):48-54.
- Duncan M, Warden P, Bernatchez SF, Morse D. A bundled approach to decrease the rate of primary bloodstream infections related to peripheral intravenous catheters. Journal of the Association for Vascular Access. 2018;23(1):15-22.
- 3M data on file TECH-REPORT-05-742819









